Today we live in a world of full of environmental toxicity and potential toxic exposures. Every inch of the planet has been exposed to some human tampering that has affected the air, water, soil, climate, food supply, homes, and businesses. There is no doubt that Americans live in a toxic world, on a scale never seen before in human history.
The most vulnerable members of our society, our children, are beginning to show this toxic burden through the development of terminal and chronic illnesses.
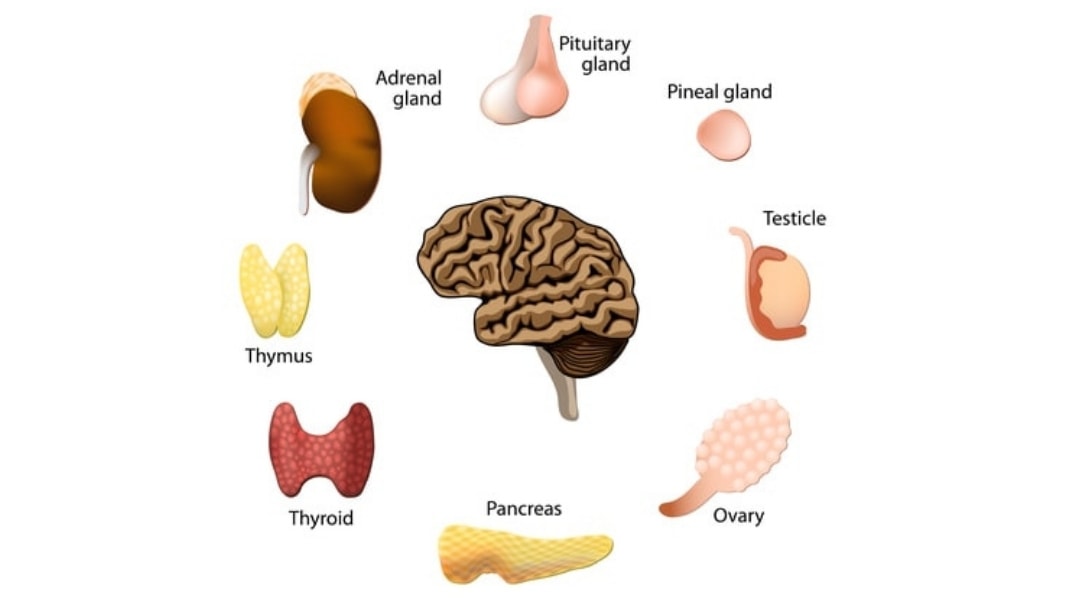
Toxins Harm Cells and Tissues
There are two main concerns with children’s exposure to environmental toxins. First, certain toxins can be extremely harmful to cells and tissues of the body. For instance, mercury, ubiquitous in our environment, is a known neurotoxin that can cause neurodevelopmental delays and dysfunction. It is in our air, our water, and even our soil and food.
Children with chronic illnesses have been found to have high levels of heavy metals, petroleum-based chemicals and a variety of other damaging toxins in their bodies.
Toxins Harm the Gastrointestinal System
Second, many toxins act directly on the gastrointestinal system, harming the colonies of good bacteria in the gut. For instance, mercury, fluoride, and chlorine are all known to adversely affect the good bacteria in our gut. The good bacteria are an essential part of our bodies’ detoxification process. Friendly bacteria, for example, help to demethylate mercury (make it less harmful) in our bodies.
When environmental toxins assault these good bacteria, they are essentially compromising the immune system of their host, leaving them vulnerable to further toxic and infectious assaults.
Toxic exposure can result in significant immune dysregulation (often seen as autoimmunity), combined with cellular and tissue damage.
Common Toxins
Some of the most common toxins include:
- Arsenic
- Mercury
- Aluminum
- Lead
- Fluoride
- Cadmium
- Pesticides
- Plastics
- BPA
- Phthalates
- Solvents
- Mold
- Mycotoxins
- Endotoxins
- Bromine
- Carcinogens
- Endocrine disruptors
- PCBs
- DDT
- PBDEs and other flame retardants
- Electromagnetic fields (EMFs)
Since the time of the industrial revolution, progress has polluted our environment to the point that now not only our environment has been severely and tragically affected, but also our most precious legacy: our children.
Environmental toxicity has had a direct impact on the physical and neurological development of our children today. It is, therefore, no surprise we have “canaries in the coal mine” and unheard of epidemics such as autism spectrum disorders, asthma, diabetes, allergies and so on which were rarely seen 50 years ago.
How Does Environmental Toxicity Affect Our Children?
It is a well-known fact that children experience a much stronger impact from environmental toxicity than adults.
- The blood-brain barrier in a child is much porous than adults, and therefore, more vulnerable to having chemical exposures reaching the developing brain. Children also have lower levels of some chemical binding proteins which allow more toxins to affect their organs. Many children exposed to environmental toxicity at an early age and/or in utero may have their neurological, immune, sensory and nervous systems affected which now becomes a more complicated and complex process such as autism spectrum disorders.
- Many children carry a genetic variant defect called MTHFR which results in reduced glutathione. Glutathione is the master antioxidant in the body which aids the body in excreting toxicity to keep a healthy body, mind and spirit. Children carrying the genetic mutation MTHFR would carry far greater risks to environmental toxicity than children without.
Researchers now know that exposures to environmental contaminants are cumulative and may have generational effects still to come.
What Can We Do to Protect Our Children?
- Green your home: Buy organic produce, meats, fruits and free-range non GMO (genetically modified organism) without pesticides and growth hormones to feed your family.
- Buy only wild fish, not farm raised; avoid fish with mercury and use pure fish oil without mercury as well.
- Avoid all process and prepackaged foods and eliminate all artificial sweeteners, dyes, MSG, aspartame, toxic preservatives and eat freshly cooked or raw foods.
- Store your food and beverages in glass rather than plastic and avoid plastic wrap and canned foods that have BPS and BPA.
- Use a water filter for drinking water and even for your shower or bath.
- Clean your home with natural cleaning products.
- Buy natural brands of toiletries, shampoos, toothpaste, deodorants, cosmetics and soaps.
- Avoid using artificial air fresheners, dryer sheets, fabric softeners, dish washer cleaners and synthetic fragrances – use essential oils instead.
- Replace your non-stick and aluminum pots and pans and replace with glass, ceramic, and other natural cookware.
- Use natural pesticide and insect repellents.
- Reduce the usage of drugs and medication: choose natural supplements, homeopathy, herbs and essential oils for your children’s health and wellness.
- Reduce the toxic electromagnetic smog in your house – shut off your WiFi.
- Review our checklist for greening your home.
Still Looking for Answers?
Visit the Epidemic Answers Practitioner Directory to find a practitioner near you.
Join us inside our online membership community for parents, Healing Together, where you’ll find even more healing resources, expert guidance, and a community to support you every step of your child’s healing journey.
Sources & References
Adams, J.B., et al. Mercury in first-cut baby hair of children with autism versus typically-developing children. Toxicological & Environmental Chemistry. 2007 Jun;70(12):1046-51.
Adams, J.B., et al. Mercury, Lead, and Zinc in Baby Teeth of Children with Autism Versus Controls. Journal of Toxicology and Environmental Health. 2007 Jun;70(12):1046-51.
Alampi, J.D., et al. Gestational Exposure to Toxicants and Autistic Behaviors using Bayesian Quantile Regression. Am J Epedemiol. 2021 Sep 1;190(9):1803-1813.
Aldad, T.S., et al. Fetal Radiofrequency Radiation Exposure From 800-1900 Mhz-Rated Cellular Telephones Affects Neurodevelopment and Behavior in Mice. Sci Rep. 2012;2:312.
Banks, W.A., et al. Aluminum-induced neurotoxicity: alterations in membrane function at the blood-brain barrier. Neurosci Biobehav Rev. 1989 Spring;13(1):47-53.
Bernard, S., et al. Autism: a novel form of mercury poisoning. Med Hypotheses. 2001 Apr;56(4):462-71.
Mixtures of persistent organic pollutants are found in vital organs of late gestation human fetuses. Chemosphere. 2021 Nov;283:131125.
Braun, J.M., et al. Association of Environmental Toxicants and Conduct Disorder in U.S. Children: NHANES 2001-2004. Environ Health Perspect. 2008 Jul;116(7):956-62.
Braun, J.M., et al. Exposures to environmental toxicants and attention deficit hyperactivity disorder in U.S. children. Environ Health Project. Dec 2006;114(12):1904-1909.
Choi, A.L., et al. Developmental Fluoride Neurotoxicity: A Systematic Review and Meta-Analysis. Environ Health Perspect. 2012;120(10).
Cohen, Patricia. Roundup Maker to Pay $10 Billion to Settle Cancer Suits. The New York Times. 24 Jun 2020.
Deisher, T.A., et al. Impact of environmental factors on the prevalence of autistic disorder after 1979. J Public Health and Epidemiology. Sep 2014;6(9):271-286.
Deth, R., et al. How environmental and genetic factors combine to cause autism: A redox/methylation hypothesis. Neurotoxicology. 2008;29(1):190-201.
Environmental Working Group. Body Burden: The Pollution in Newborns. 14 Jul 2005.
Geier, M.R., et al. The potential importance of steroids in the treatment of autistic spectrum disorders and other disorders involving mercury toxicity. Med Hypotheses. 2005;64(5):946-54.
Grandjean, P., et al. Developmental neurotoxicity of industrial chemicals. Lancet. 2006 Dec 16;368(9553):2167-78.
Gunatilake, S., et al. Glyphosate’s Synergistic Toxicity in Combination with Other Factors as a Cause of Chronic Kidney Disease of Unknown Origin. Int J Environ Res Public Health. 2019 Jul 31;16(15):2734.
Hansen, J.B., et al. Prenatal exposure to bisphenol A and autistic- and ADHD-related symptoms in children aged 2 and5 years from the Odense Child Cohort. Environ Health. 2021 Mar 12;20(1):24.
Hanson, D.R., et al. Theories of schizophrenia: a genetic-inflammatory-vascular synthesis. BMC Medical Genetics. 2005 Feb 11;6:7.
Harley, K.G., et al. Changes in Latina Women’s Exposure to Cleaning Chemicals Associated with Switching from Conventional to “Green” Household Cleaning Products: The LUCIR Intervention Study. Environ Health Perspect. 2021 Sep;129(9):97001.
Hauser, P., et al. Resistance to thyroid hormone: implications for neurodevelopmental research on the effects of thyroid hormone disruptors. Toxicol Ind Health. 1998 Jan-Apr;14(1-2):85-101.
Herbert, M.R., et al. Autism and environmental genomics. Neurotoxicology. 2006;27(5):671-84.
Herbert, M.R., et al. Autism and EMF? Plausibility of a pathophysiological link part I. Pathophysiology. 2013 Jul;1-19.
Herbert, M.R., et al. Autism and EMF? Plausibility of a pathophysiological link part II. Pathophysiology. 2013 Jun;20(3):211-34.
Hertz-Picciotto, I., et al. Organophosphate exposures during pregnancy and child neurodevelopment: Recommendations for essential policy reforms. PLoS Med. 2018 Oct 24;15(10):e1002671.
Hertz-Picciotto, I., et al. Polybrominated diphenyl ethers in relation to autism and developmental delay: a case-control study. Environ Health. 2011 Jan 5;10(1):1.
Hertz-Picciotto, I., et al. Prenatal exposures to persistent and non-persistent organic compounds and effects on immune system development. Basic Clin Pharmacol Toxicol. 2008 Feb;102(2):146-54.
Hinhumpatch, P., et al. Oxidative DNA damage and repair in children exposed to low levels of arsenic in utero and during early childhood: application of salivary and urinary biomarkers. Toxicol Appl Pharmacol. 2013;273(3):569-79.
Holmes, A., et al. Reduced Levels of Mercury in First Baby Haircuts of Autistic Children. International Journal of Toxicology. Jul-Aug 2003;22(4):277-85.
Jafari, M.H., et al. The Relationship Between the Level of Copper, Lead, Mercury and Autism Disorders: A Meta-Analysis. Pediatric Health, Medicine and Therapeutics. 21 Sep 2020(11):369—378.
Jafari, T., et al. The association between mercury levels and autism spectrum disorders: A systematic review and meta-analysis. J Trace Elem Med Biol. 2017 Dec;44:289-297.
Jedrychowski, W., et al. COGNITIVE FUNCTION OF 6-YEAR OLD CHILDREN EXPOSED TO MOLD-CONTAMINATED HOMES IN EARLY POSTNATAL PERIOD. PROSPECTIVE BIRTH COHORT STUDY IN POLAND. Physiol Behav. 2011 Oct 24; 104(5): 989–995.
Jett, D.A. Chemical toxins that cause seizures. Neurotoxicology. 2012 Dec;33(6):1473-5.
Johansson, O., et al. Exacerbation of demyelinating syndrome after exposure to wireless modem with public hotspot. Electromagn Biol Med. 2016;35(4):393-7.
Julvez, J., et al. Early life multiple exposures and child cognitive function: A multi-centric birth cohort study in six European countries. Environ Pollut. 2021 Sep 1;284:117404.
Kern, J.K., et al. A biomarker of mercury body-burden correlated with diagnostic domain specific clinical symptoms of autism spectrum disorder. Biometals. 2010;23(6):1043-51.
Konkel, L. Phthalates and Autistic Traits: Exploring the Association between Prenatal Exposures and Child Behavior. Environ Health Perspec. 2020 Oct;128(10):104001.
Landrigan, P.J., et al. Children’s vulnerability to toxic chemicals: a challenge and opportunity to strengthen health and environmental policy. Health Aff. (Millwood). 2011 May;30(5):842-50.
Lanphear, B.P., et al. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ Health Perspect. 2005;113(7).
Lathe, R. Environmental factors and limbic vulnerability in childhood autism; Clinical report. American Journal of Biochemistry and Biotechnology. 4 (2): 183-197, 2008.
Lombardi, C., et al. Residential proximity to pesticide application as a risk factor for childhood central nervous system tumors. Environ Res. 2021 Jun;197:111078.
Lyall, K., et al. Prenatal Serum Concentrations of Brominated Flame Retardants and Autism Spectrum Disorder and Intellectual Disability in the Early Markers of Autism Study: A Population-Based Case-Control Study in California. Environ Health Perspect. 2017 Aug 30;125(8):087023.
Messer, A. Mini-review: polybrominated diphenyl ether (PBDE) flame retardants as potential autism risk factors. Physiol Behav. 2010 Jun 1;100(3):245-9.
Napoli, E., et al. Toxicity of the flame-retardant BDE-49 on brain mitochondria and neuronal progenitor striatal cells enhanced by a PTEN-deficient background. Toxicol Sci. 2013 Mar;132(1):196-210.
Palmer, R.F., et al. Environmental mercury release, special education rates, and autism disorder: an ecological study of Texas. Health Place. 2006(12):203-209.
Palmer, R.F., et al. Proximity to point sources of environmental mercury release as a predictor of autism prevalence. Health and Place. 2009 Mar;15(1):18-24.
Rauh, V.A., et al. Impact of prenatal chlorpyrifos exposure on neurodevelopment in the first 3 years of life among inner-city children. Pediatrics. 2006;118;e1845-1859.
Rowland, I.R., et al. Effects of diet on mercury metabolism and excretion in mice given methylmercury: role of gut flora. Archives of Environmental Health. Nov-Dec 1984;39(6):401-8.
Samsel, A., et al. Glyphosate, pathways to modern diseases II: Celiac sprue and gluten intolerance. Interdiscip Toxicol. 2013 Dec;6(4):159-84.
Samsel, A., et al. Glyphosate, pathways to modern diseases III: Manganese, neurological diseases, and associated pathologies. Surg Neurol Int. 2015 Mar 24;6:45.
Samsel, A, et al. Glyphosate’s suppression of cytochrome P450 enzymes and amino acid biosynthesis by the gut microbiome: Pathways to modern diseases. Entropy. 2013;15:1416–1463.
Song, Y., et al. Effects of acute exposure to aluminum on blood-brain barrier and the protection of zinc. Neurosci Lett. 2008 Nov 7;445(1):42-6.
Tang, J., et al. Exposure to 900 MHz electromagnetic fields activates the mkp-1/ERK pathway and causes blood-brain barrier damage and cognitive impairment in rats. Brain Res. 2015 Mar 19;1601:92-101.
Thompson, L., et al. What have birth cohort studies asked about genetic, pre- and perinatal exposures and child and adolescent onset mental health outcomes? A systematic review. Eur Child Adolesc Psychiatry. 2010;19(1):1-15.
U.S. Food and Drug Administration. FDA Issues Recommendations for Certain High-Risk Groups Regarding Mercury-Containing Dental Amalgam. 24 Sep 2020.
Wallinga, D., et al. Not So Sweet: Missing Mercury and High Fructose Corn Syrup. Institute for Agriculture and Trade Policy, Minneapolis, Minnesota. Jan 2009.
Wang, H.L., et al. Case-Control Study of Blood Lead Levels and Attention Deficit Hyperactivity Disorder in Chinese Children. Environmental Health Perspectives. 2008 Oct;116(10):1401-6.
Windham, G.C., et al. Autism Spectrum Disorders in Relation to Distribution of Hazardous Air Pollutants in the San Francisco Bay Area. Environmental Health Perspectives. 2006 Sep;114(9):1438-44.
Wong, S., et al. Autism, Mitochondria and Polybrominated Diphenyl Ether Exposure. CNS Neurol Disord Drug Targets. 2016;15(5):614-23.
Resources
Articles
The Environmental Working Group. Body Burden: The Pollution in Newborns. 14 Jul 2005.
Swan, Shanna, et al. Reproductive Problems in Both Men and Women Are Rising at an Alarming Rate: A likely culprit is hormone-disrupting chemicals. Scientific American, 16 Mar 2021.
Books
Fitzgerald, Randall. The Hundred-Year Lie: How to Protect Yourself from the Chemicals That Are Destroying Your Health. London: Plume, 2007.
Hong, Maria Rickert. Almost Autism: Recovering Children from Sensory Processing Disorder, A Reference for Parents and Practitioners. 2014.
Perro, Michelle, et al. What’s Making Our Children Sick?: How Industrial Food Is Causing an Epidemic of Chronic Illness, and What Parents (and Doctors) Can Do About It. Chelsea Green Publishing, 2017.
Rogers, Sherry. Detoxify or Die. Prestige Publishing, 2002.
Wachter, Kenneth W., et al. Offspring: Human Fertility Behavior in Biodemographic Perspective. National Academy of Sciences, 2003.
Videos
A Global Fertility Crisis – Dr. Shanna Swan